Our greatest glory is not in never failing, but in rising up every time we fail.
Ralph Waldo Emerson

Depression is a common and serious mental health condition. It affects how we think, feel, and do our normal daily activities.
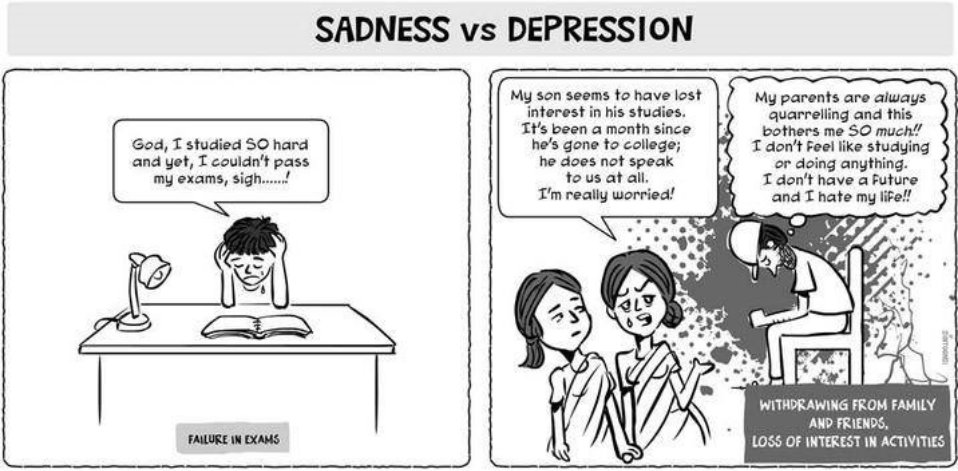
Depression is often confused with sadness. When one has depression, they are in a very low state. It is more than sadness and people with depression are not themselves. Many people go through depression without their friends or family even knowing.
It’s no secret that there is a strong connection between substance use and mental illness. The National Bureau of Economic Research reports that individuals with a history of mental illness are 25% more likely to consume alcohol, 69% more likely to consume cocaine, and 94% more likely to consume cigarettes. When a person struggles with substance misuse and a mental illness, this is known as a dual diagnosis or co-occurring disorder.
Mood disorders, especially major depressive disorder (MDD) and bipolar disorder (BD), often coincide with substance use disorders (SUDs). Prevalence of substance use disorders in people with BD ranges from 20% to 70% and from 10% to 30% in persons with MDD. Alcohol use disorder is the most common SUD in individuals with BD, occurring in about 42%, and cannabis use disorder is the next most common, at about 20%.
Depression is a mental illness frequently co-occurring with substance use. The relationship between the two disorders is bi-directional, meaning that people who misuse substances are more likely to suffer from depression and vice versa. People who are depressed may drink or use drugs to lift their mood or escape from feelings of guilt or despair. But substances like alcohol, which is a depressant, can increase fatigue which affects concentration, inhibitions, decision-making, and reaction times.
Comprehensive treatment is available for both depression and substance use and is usually the best course of action. Antidepressants can do a great deal to reduce depressive symptoms and some medications are available to treat alcohol use disorder, opioid use disorder, and others. Research shows that medication frequently is more effective when an individual seeks counseling and behavioral support as well. Many people find that intensive outpatient or inpatient treatment is necessary to curb addiction and learn healthy coping strategies for depression.
When seeking treatment for substance use and depression, you first may need to seek immediate medical attention to address the withdrawal symptoms of drugs or alcohol. Some period of abstinence may be necessary before a clinician can conduct an accurate diagnostic assessment. Talk to your doctor about programs that address the dual diagnoses simultaneously. If you simply end the substance use, which has largely served as a way of coping with depression, then your depression may worsen and increase your risk of relapse.
Some with a dual diagnosis can cope well with counseling, medical support, and peer support for addiction. Others may find that intensive inpatient or outpatient treatment programs work best. Effective treatment approaches are long-term and multimodal, aimed at reducing length, frequency, and severity of substance use while simultaneously improving health and quality of life.
A comprehensive treatment program typically includes medical and psychiatric care, counseling, case management, and peer support groups, as well as access to support for vocational, legal, financial, housing, transportation, and childcare needs.
While relapse may and often occurs, people generate the greatest odds for long-term recovery when they treat both the depression and the substance use.
If you have been diagnosed with depression, talk to your doctor about the risk of substance use. You may want to closely monitor your intake of alcohol and seek alternative coping strategies for stress and low mood. If you have an active substance use disorder or a history of substance use, it’s possible that you have undiagnosed depression. A combination of regular communication with your physician, counseling, and peer support can help you develop protective coping skills to reduce the risk of relapse or developing depression.
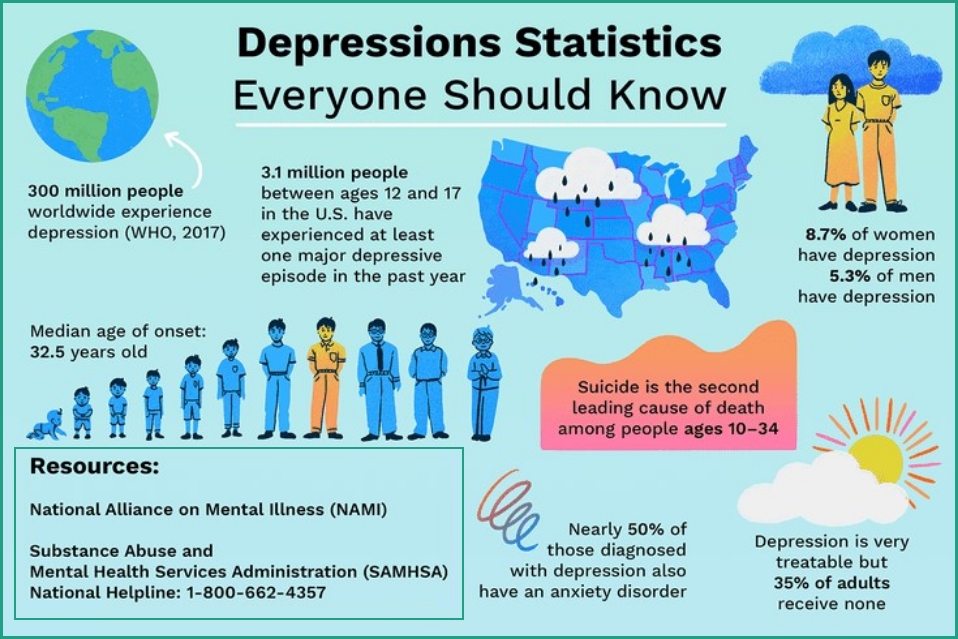
Depression is more common than people realize. Below are some depression statistics everyone should know.
The symptoms are different for everyone and each person deals with it differently. However, common symptoms are:
Depression can happen to anyone. Look out for signs and be observant of your friends and family. If you know someone who may have depression, try to approach them in a cautious yet extremely caring way. They may try to avoid the topic or the observation that they seem different. When you know someone is depressed, do not put them down. For example, saying “snap out of it” or “I’m tired of hearing this.” They need someone who will listen and be kind to them whether they realize it or not. Be there for them, just asking them how they are doing is a great support.






The symptoms are different for everyone and each person deals with it differently. However, common management techniques are:
The most important thing to remember is you are not alone.